
Sleep is an essential part of a healthy lifestyle. Lack of sleep has been shown to cause an increase in blood pressure, decreased concentration and forgetfulness, increases the speed of aging, leads to depression and weight gain. For patients, sleep is especially important for recovery.
As a physical therapist or other travelling healthcare professional, how can you help your patients (and yourself) get a better night of sleep?
As an integral part of the initial evaluation, the PT should always ask the patient about their sleep and then follow up with education and self-care/home management tips to facilitate a faster recovery.
Many issues that contribute to sleep difficulties include pain and lack of bed mobility. Without adequate rest and recovery, patient illness and suffering can be prolonged, and your own lack of adequate rest can lead to less-than-ideal work performance.
Ask specific questions regarding sleep. For example, does the pain affect a patient’s ability to fall asleep and or stay asleep? Does the patient wake multiple times per night?
Address difficulty falling asleep (unrelated to pain) by educating the patient to avoid caffeine later in the day, minimizing alcohol use, and reducing screen time before bed. As a physical therapist, it is important to note that many of us complete our documentation at the end of day. If you are having trouble getting to sleep yourself, find ways to complete documentation while at work. Practicing “belly” or “abdominal breathing” is a good way to help relax and unwind when you first get into bed.
To perform belly breathing, find a comfortable position in your bed, breathe in through your nose slowly for 4-5 seconds while allowing the belly to rise, then breathe out through “pursed lips” for 4-6 seconds as the belly pulls in. Repeat this 3-5 minutes, with slow and easy breaths. Concentrate only on the breath, and push all thoughts out of your mind. As with any activity, practice will improve your ability to relax.
Then identify the size, age, and quality of the patient’s matrices. Is the mattress too soft? Does it dip in the middle? Does the patient sleep with a snoring partner, or a bed hogging child and/or pets?
It can be difficult getting patients (and yourself!) to change habits, especially when family members contribute to sleep deprivation.
Suggestions to combat this include temporarily sleeping in another room, getting ear plugs, and transitioning children and pets into their own beds – or purchasing a bigger and/or more supportive mattress.
Next, educate patients on proper positioning to support the spine and extremities to reduce pain provocative positions. For example, belly sleeping causes end range neck rotation and hyper lumbar extension, which would be the equivalent of bending backwards for four to eight hours. Semi-stomach sleepers introduce prolonged lumbar side bending. Sleeping straight on the back increases nerve tension leading to lower back pain.
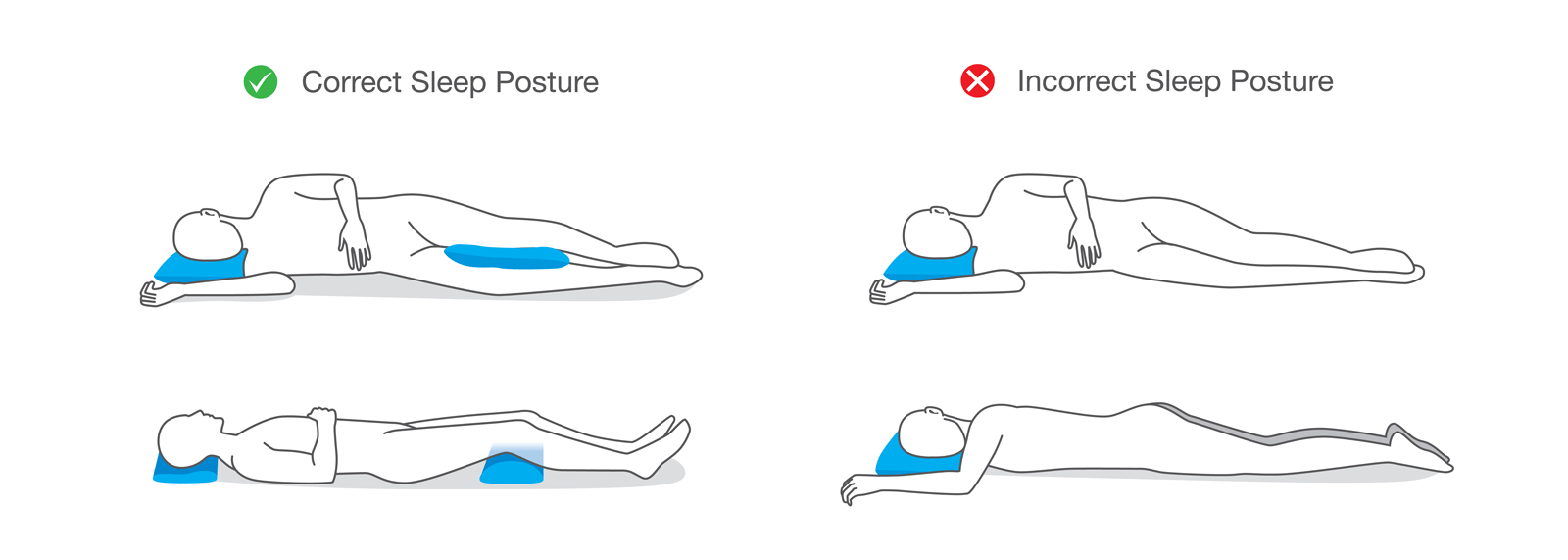
For back sleepers, teach the patient to place a pillow or a wedge under the knees large enough to reduce lower back hyper-extending and slacken nerve tension. The neck pillow should be under the head, not under the upper back and must be big enough to accommodate a patient with a curved upper back but not so large that it makes it difficult to breath by bringing the chin to the chest.
Side sleeping is best for patients with back and neck pain. Suggest they sleep on the unaffected side for those with shoulder and hip pain. To achieve a straight spine in side lying, place a pillow under the head and a towel under the neck for additional support the neck. To keep the back in a neutral, place another towel in the “hourglass curve”. Patients with shoulder pain will benefit from a “hug” pillow and all patients benefit from a pillow between their knees and another between the feet.
Once all of the pillows and towels are placed, have the patient play with the amount of neck flexion and extension as well as hip and knee flexion to minimize pain. Have the patient try “pillows and towels” in the clinic. Once comfortable, take one towel or pillow away at a time so they can feel the difference of sleeping with a supported neural spine.
Follow up with the patient on their next visit to see if they had any success with these recommendations. Most will complain about the pillows and towels, and report that it is difficult to roll, which of course, is true. But remind them that they will sleep better, which will facilitate a faster recovery, and as they feel better, they will eventually be able to sleep without the support.

